Background
For many patients, carers and service users, the pandemic has caused a shift from co-production back to a more prescriptive style of interaction with healthcare professionals. We will look at this shift, and how it’s more important than ever that patients have a voice.
Sessions and speakers
A7: Co-producing improvements in experience and quality: the WHY and the HOW
Fiona Godlee, The BMJ; England
David McNally, NHS England/NHS Improvement; England
Cristin Lind, Healthcare advocate; Sweden
Vibeke Rischel, Danish Society for Patient Safety; Denmark
Jane McGrath, WeCoproduce; England
We started our co-production journey by reflecting on how the pandemic has affected us. Not surprisingly, around 75% of the audience said that COVID-19 has made co-production more difficult. So we focused this session on what we can do to address this.
A key loss in working remotely is the interaction with other human beings. For some of us, this has highlighted just how important it is to get affirmation and support from our colleagues. We must also remember to GIVE that affirmation too. Don’t be shy to show your appreciation of others.
We can go some way to restoring this connection by just picking up the phone and giving someone a ring. An informal chat can provide a lot of the support and communication that might be lost in a Zoom meeting.
There’s a strong thread of self-care through all of this. Jane McGrath of WeCoproduce shared this frankly genius “map” of COVIDland. The pandemic has created a lot of difficult emotions, around tensions in evidence-based care and fear and anger due to the exclusion of family members from care. Where are you on this landscape?
The huge changes in working practices exacerbate problems in connecting with patients. Many are not able to use digital technology to engage with co-production. Can co-production keep up with the break-neck pace demanded by senior management? We heard from David McNally about a successful, rapid development of a national musculoskeletal strategy. But we also heard from others that funding and support for co-production has disappeared.
Let’s look at some of the opportunities
Of course, digital technology, although a barrier for some, opens up channels to others, especially younger participants. New media mean new opportunities. One group created a radio station – gagaradio, another uses a simple Facebook group to keep people updated and facilitate discussion. The key challenge is how you create a platform in which the right interactions can take place.
How are you creating “welcome”?
Think about what you are doing to make people feel welcome in your digital meeting or event. Take time to have them introduce themselves, and consider using ice-breakers. Maybe they can locate themselves on Jane’s map! Some people are using music and poetry to soften the edges before a meeting. Others just open the meeting up half an hour early so people can drift in and chat just like they would do in a face-to-face meeting.
There are things we can do to try to manage changed work patterns, but we also need to keep the pressure up to ensure that co-production is properly resourced. Case in point – Cristin Lind illustrated the “command and control” style of much COVID-related public information, and raised the question of whether co-production could have helped to produce better messages, that resulted in more engagement.
B4: Co-production and beyond: patients leading the way
On Tuesday, we enjoyed four rapid-fire video presentations describing the global shift from co-production to patient-led improvement and demonstrating the benefits of getting patients involved at every level of an organisation. At a time when it is easy to be caught up in the moment, it is very helpful to reflect on what good co-production looks like and why it matters so much.
A seat at the table: Transforming healthcare with patient-executive partnerships
Patrice Daquin and Frank Licciardi, Memorial Sloan-Kettering Cancer Care (MSK), USA
MSK is one of the biggest cancer care organisations in the US. They established a Patient and Family Advisory Council for Quality to help integrate patient perspectives into every aspect of the mission. Patrice and Frank describe how they achieved this in areas as diverse as a Patient Values tab for electronic health records, discharge planning and service transformation for dying patients.
You can’t have advisors travel with you on your journey unless they become part of the expedition team.
Structures for patient involvement and co-production
Louise Patmore, Sussex Partnership NHS Trust, England
In her presentation, Louise describes how moving from patient involvement to leadership, the Trust ensures that the service user and carer voice is at the heart of Trust’s strategic work.
A key step was the creation of a “Participation Directorate” to oversee involvement activities across a range of settings and services. This also facilitates connections with local authorities, emergency services and other health services, as well as third sector community organisations. Allied with a focus on participation culture, the group is now developing a network of teams.
Divergent patient and provider value-based healthcare experiences: the ‘Big Bang Theory’ solution
Marion George and Katharina Kovacs Burns, Alberta Health Services, Canada
Marion and Katharina talked about a study they are conducting of patient and public involvement in Alberta, a health system of over 4 million people. By co-designing this study they brought together diversity of opinions and cultures. They were able to demonstrate with evidence that improvement had a positive effect on outcomes. This led to clear understanding of “what matters most” from the patients’ perspectives.
Co-production of care: engaging patients in service improvement and pathway design
Comfort Adeosun, Quality Improvement team lead, Ministry of Defence, Nigeria
Comfort describes her experiences in a setting where the value of patient involvement and participation was not well known at the outset. She presented the theory that If we engage patients in redesigning pathways, we will reduce waiting time, improve patient satisfaction and hospital performance. Each QI project had clear outcome measures, including qualitative data from both patients and providers. The target of 20% reduction in waiting time was achieved within 3 months. 18 months later, it had been reduced by 80%, and led to further process improvements and ongoing changes to care pathways.
C7: Patient centric research during the pandemic: Keeping the wheels turning
Emma Doble & Henry Scowcroft, BMJ; UK
Sara Riggare, Uppsala University, Sweden
Athena Akram, University College London, UK
Hannah Davis, Independent researcher, USA

The pandemic has severely disrupted research activities across the board. Henry commented that patient groups have been left out of the pandemic. Patient involvement groups have stopped meeting. There have been wholesale changes to health services without patient voices being in the room. Judging by the comments from the other participants, he is not alone in this view.
That said, many groups have made efforts to keep going, for example by working with researchers to develop online study recruitment methods. However, there is no doubt that patient-led research.
The gold standard of PPI in research is where patients, especially those with long-term conditions, actually become researchers themselves. And guess what? The pandemic has spawned some outstanding examples of patients doing it for themselves.
Hanna Davis and Athena Akram gave a fascinating account of developing an online community of “Long COVID” sufferers. Already being patient activists, and a bit handy with digital technology, they used Slack to set up a multi-channel discussion forum for working with these people.
They captured and surveyed symptoms, provided to support to sufferers, and, crucially, reported their findings to the powers that be. The NIH blogged about their work, and they presented it to the WHO. In collaboration with UCL (London) they now have a comprehensive, IRB-approved survey under way. Their aims now are to:
- Acknowledge that Long-COVID is a real illness
- Get an estimate of its prevalence
- Give advice on basic symptom management
- Provide a caring and inclusive environment for discussion
- Promote aggressive research into the pathophysiology of Long COVID.
Of course, not everyone hits the ground running as a fully fledged patient-researcher and digital-influencer. We are reminded of the importance of developing the skills amongst patient researchers, nicely summarised in this slide by Sara Riggare. You can read more on her blog.
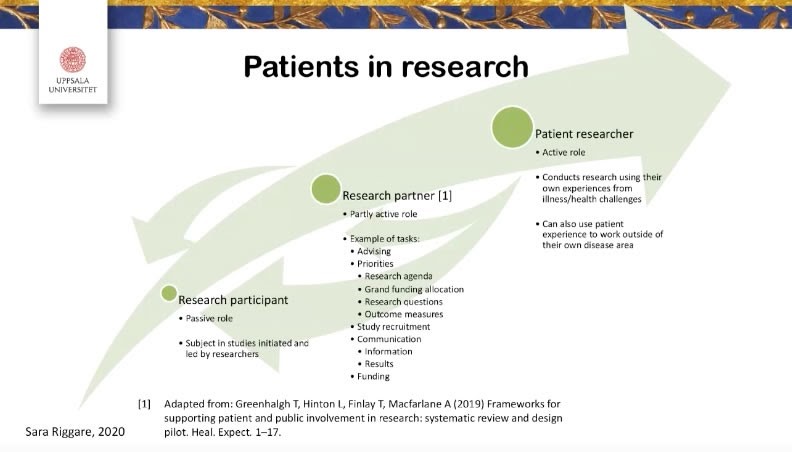
Experienced patient researchers can and should help new people to increase their knowledge, skills and confidence in being active participants in research.
So it seems that although research has taken a huge hit during the pandemic, in some areas patients have taken the lead to fill this vacuum. Nothing better illustrates the huge potential of co-production. Health professionals have faced enormous challenges in reconfiguring services. The key message I take from this conference is that patients are allies in meeting the challenge, not problems to be dealt with.
Ask them, empower them and support them. We will all benefit!
D4: What Matters to You? – sharing experience from 4 countries
Damara Gutnick, Montefiore Hudson Valley Collaborative (MHVC) and Albert Einstein School of Medicine; USA
Karen Turner, Royal Free London NHS Foundation Trust; England
Anders Vege, Norwegian Institute of Public Health; Norway
Shaun Maher, Scottish Government; Scotland
Tommy Whitelaw, Carer; Scotland
Maureen Bisognano, Institute for Healthcare Improvement (IHI); USA

We took up this theme by revisiting one of the most important cornerstones of quality improvement, co-production and public involvement. Ask, and listen. Tommy got us started with a very moving and frank account of his experiences caring for his mother, who had vascular dementia. His message is “Know the person, and understand what matters to them”. He has since helped establish the worldwide What Matters to You movement, now responsible for over 30,000 conversations oriented around improving care.
We heard similar stories from Maureen and Anders. As a health care outsider, it’s shocking to me that there needs to be a “What Matters to You” movement at all. But when you consider the context of services that are structured around specialties, a chronic lack of time and the pressure to “do the right thing for the patient”, perhaps it’s not so surprising.
Sometimes clinicians and other health professionals can be reluctant to ask this question of patients. In part, this is because they know the answers may be beyond their capacity to help: social issues, family concerns or even just practical worries such as being evicted from rented accommodation.
The same is often true of health professionals themselves. The question is seldom posed to them, because managers “know” that they can’t do anything about the answers (lack of time, lack of resources etc.) Karen took us through her experiences of using that question to initiate a “Joy-at-work” approach to improving ICU services at the Royal Free Hospital in London. Health care managers can take heart from her findings of the impact on staff turnover.
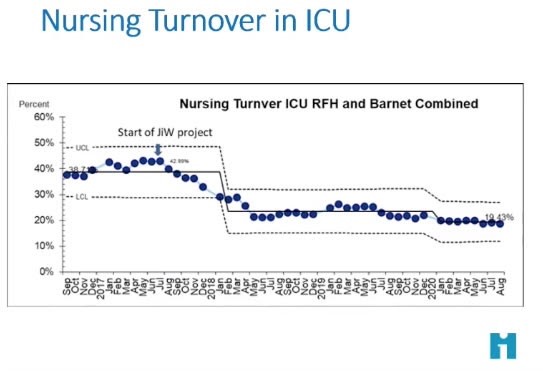
Here’s a handy slide for the next time someone says to you “Oh I don’t have time for any of that Joy-in-Work stuff”
So it’s important to ask What Matters to You in the right way, keep asking it and reflect on the answers together. We can recommend the useful advice, information, support and resources from Montefiore Hudson Valley Collective.
Good luck! We’re all counting on you.
Last updated: 6 November 2020, 16:36 GMT
Author: Douglas Badenoch, Beyond the Room
SHARE THE BLOG:


